Human serum albumin
Human Serum Albumin: A key to advances in personalized medicine and targeted drug delivery.
Human Serum Albumin: A key to advances in personalized medicine and targeted drug delivery.
Modern medicine is at a turning point where personalized approaches and targeted therapies are gaining prominence. This shift is driven by the need to develop more efficient, safer, and patient-specific treatment strategies. At the heart of this movement is Human Serum Albumin (HSA), a versatile protein that serves not only as a transport molecule in our blood but also as a promising carrier for drugs in targeted drug delivery systems.
What is HSA?
HSA is the most abundant protein in human blood plasma, accounting for about 50-60% of the total protein content. It is synthesized in the liver and performs a variety of functions within the body. Its primary role is to act as a transport medium for various endogenous and exogenous substances such as fatty acids, hormones, bilirubin, metabolites, and medications. Additionally, HSA plays a crucial role in maintaining colloid osmotic pressure and regulating blood pH levels.
Structure and Properties
HSA is a single-chain protein with a molecular weight of approximately 66.5 kDa. It consists of 585 amino acids, forming a stable, three-dimensional structure reinforced by 17 disulfide bridges. This structure imparts exceptional stability and solubility to HSA, even under extreme conditions of pH, temperature, and chemical influences.
One of the most notable properties of HSA is its ability to bind a wide range of ligands. This is enabled by the presence of specific binding sites on the protein surface, which exhibit high affinity for various molecules. This binding capacity makes HSA an ideal candidate for use as a carrier molecule in drug delivery.
Personalized Medicine: A paradigm shift
Personalized medicine, also known as precision medicine, aims to take into account the individual differences in genetics, lifestyle, and environment of the illness of a patient to develop tailored treatment approaches. This method contrasts with the traditional “one-size-fits-all” strategy, where a treatment is applied to a broad patient population regardless of individual differences.
Foundations of personalized medicine
Personalized medicine is based on the understanding that every individual is unique, not only genetically but also in terms of disease progression and response to medications. This individuality requires a customized approach that is based on the specific needs and biological characteristics of each patient.
By utilizing advanced technologies such as genome sequencing, proteomic analyses, and bioinformatics tools, doctors and researchers can gain deep insights into the molecular mechanisms of diseases and develop personalized therapies that are tailored to the specific genetic profiles and biomarkers of a patient.
Advantages of targeted drug delivery
Personalized medicine offers numerous benefits that are evident across various aspects of patient care.
- i) Since treatments are tailored to the individual genetic and molecular characteristics of the patient, there is a higher likelihood of their effectiveness. This targeted therapeutic approach ensures that patients receive exactly the medications and dosages that are best suited to their specific disease expression.
- ii) Personalized therapies minimize the risk of adverse effects since they are tailored to the specific physiology of the patient. By customizing medications to fit an individual’s genetic makeup and metabolism, the likelihood of side effects is significantly reduced, making treatment safer for the patient.
iii) By identifying genetic-level risk factors, preventive measures can be taken before a disease manifests. This allows doctors to take proactive steps to prevent the onset or progression of diseases, potentially leading to a healthier population overall.
The role of HSA in targeted drug delivery
HSA is an excellent candidate for use in targeted drug delivery due to its unique properties. It has been demonstrated that HSA can act as a carrier molecule for a variety of therapeutic agents, including small molecules, proteins, peptides, and even DNA.
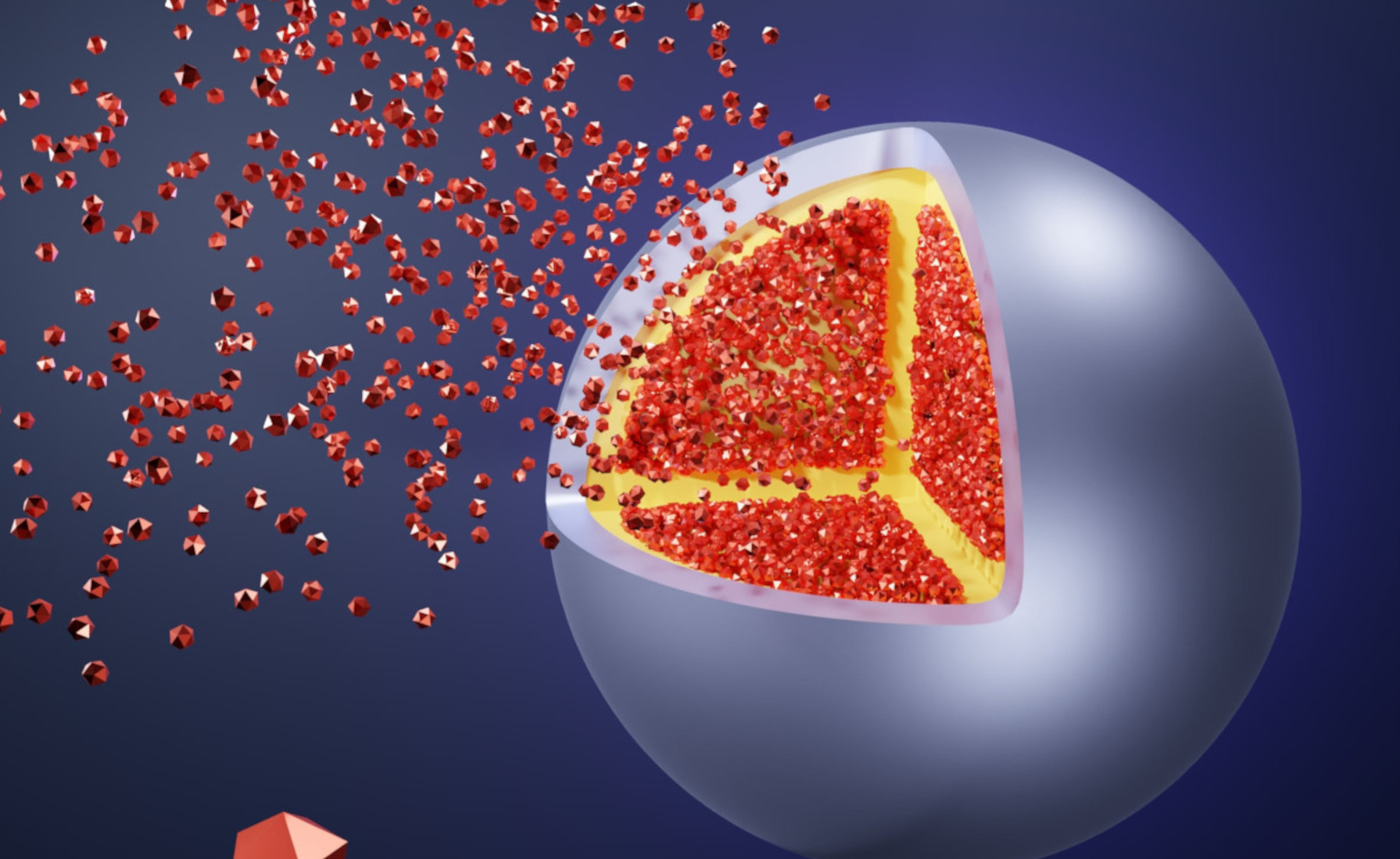
HSA as a Carrier System
Utilizing HSA as a carrier system in drug delivery offers several advantages:
- Biocompatibility: HSA is a naturally occurring protein, which means it is well tolerated by the immune system and carries a low risk of immunogenic reactions.
- Increased Half-Life: Medications bound to HSA have a prolonged half-life in the bloodstream, which enhances the effectiveness of the therapy.
- Targeted Binding: HSA can be modified to recognize and bind to specific receptors on target cells, facilitating targeted drug delivery.
- Flexibility: HSA is capable of binding a variety of therapeutic agents, enabling its use in diverse therapeutic areas.
Examples of HSA-based therapies
There are several HSA-based therapies that have been clinically tested or approved. One example is the use of HSA for delivering cancer drugs, where the albumin serves as a carrier for chemotherapeutic agents, delivering them directly to tumor cells.
Another example involves the use of HSA nanoparticles for targeted drug delivery in inflammatory diseases. These nanoparticles can specifically bind to inflamed sites in the body and deliver the medication directly to the site of inflammation. This targeted approach helps to increase the efficacy of the treatment while minimizing systemic side effects.

